FAQS
How does life coaching differ from therapy?
While both life coaching and therapy aim to support personal growth, they have distinct approaches. Therapy typically focuses on addressing past traumas, emotional healing, and diagnosing mental health conditions. On the other hand, life coaching is forward-focused, centered around setting and achieving goals, enhancing performance, and unlocking potential. If you're seeking to overcome specific challenges from your past, therapy might be more suitable. If you're looking to create a roadmap for personal or professional success, life coaching could be the right fit.
How often are coaching sessions conducted?
Coaching sessions frequency can vary based on your needs and preferences. Typically, we recommend starting with weekly sessions to establish momentum and make consistent progress. As you gain confidence and traction towards your goals, sessions might transition to bi-weekly or monthly. The flexibility of our approach ensures that the coaching frequency adapts to your evolving requirements, ensuring optimal support and accountability.
What if I'm unsure about my goals and direction?
It's completely normal to feel uncertain about your goals and direction. Our coaching process begins with an initial assessment where we'll work together to clarify your aspirations, values, and priorities. Through insightful questioning and exploration, we'll collaboratively uncover your passions and potential areas for growth. If you're not entirely sure about your goals, our coaching can help you gain clarity and chart a course that aligns with your authentic self. Remember, the journey towards clarity is an integral part of the coaching process itself.

If you or someone you know is struggling or in crisis. Help is available.
Call or text 988 Suicide & Crisis Lifeline or chat 988lifeline.org
Post-Traumatic Stress Disorder (PTSD)
Post-Traumatic Stress Disorder (PTSD) is a mental health condition triggered by experiencing or witnessing a traumatic event, such as military combat, natural disasters, serious accidents, or violent personal assaults. Individuals with PTSD may suffer from intense, disturbing thoughts and feelings related to their experience, often reliving the event through flashbacks or nightmares, and may experience severe emotional and physical reactions when reminded of the trauma. Symptoms include avoidance of reminders of the trauma, negative changes in mood and cognition, and heightened reactions like irritability or difficulty sleeping. Effective treatments for PTSD often include psychotherapy, medications, or a combination of both.
Symptoms
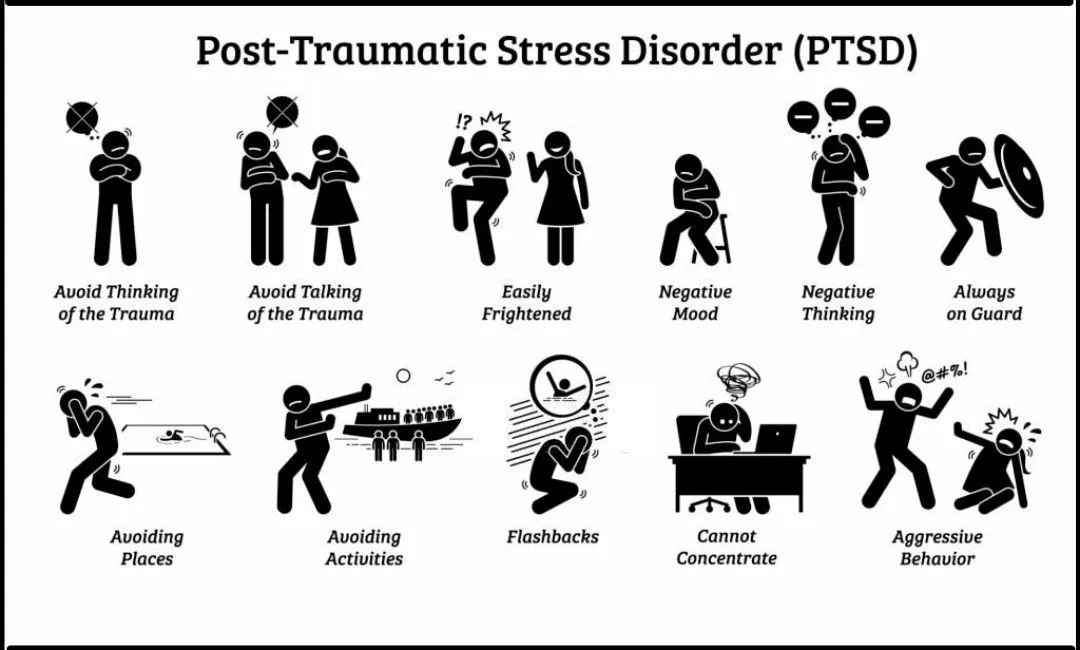
The symptoms of Post-Traumatic Stress Disorder (PTSD) can be grouped into four main categories:
1. Intrusive Thoughts: This includes recurrent, unwanted distressing memories of the traumatic event, flashbacks (reliving the trauma as if it were happening again), and nightmares related to the event. Individuals may experience severe emotional or physical reactions to reminders of the trauma.
2. Avoidance: Individuals with PTSD may avoid places, activities, or people that remind them of the traumatic event. They might also avoid discussing the trauma or their feelings about it, leading to emotional numbing and detachment from others.
3. Negative Changes in Mood and Cognition: This includes persistent negative thoughts about oneself or the world, feelings of hopelessness, memory problems (particularly surrounding the traumatic event), difficulty maintaining close relationships, and a lack of interest in activities once enjoyed. There may also be feelings of detachment or estrangement from others.
4. Alterations in Arousal and Reactivity: Symptoms in this category include being easily startled or frightened, always being on guard for danger, irritability or angry outbursts, self-destructive behavior (such as drinking too much or driving too fast), trouble sleeping, and difficulty concentrating.
These symptoms can vary in intensity and duration and may interfere significantly with your daily life, relationships, and ability to function.
Treatment Options

The best treatment options for Post-Traumatic Stress Disorder (PTSD) typically involve a combination of psychotherapy and medication. Here are the primary treatments:
1. Psychotherapy (Talk Therapy):
- Cognitive Behavioral Therapy (CBT): CBT, particularly a form called Cognitive Processing Therapy (CPT), helps individuals understand and change how they think about the trauma and its aftermath.
- Prolonged Exposure Therapy (PE): This involves repeatedly discussing the trauma in a safe environment, gradually reducing the distress associated with memories of the event.
- Eye Movement Desensitization and Reprocessing (EMDR): EMDR combines exposure therapy with guided eye movements to help individuals process and integrate traumatic memories.
- Group Therapy: Sharing experiences with others who have been through similar trauma can provide support and reduce feelings of isolation.
2. Medications:
- Selective Serotonin Reuptake Inhibitors (SSRIs): Antidepressants like sertraline (Zoloft) and paroxetine (Paxil) are commonly prescribed to help reduce PTSD symptoms.
- Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs): Medications like venlafaxine (Effexor) can also be effective.
- Other Medications: Sometimes, other medications like prazosin (to reduce nightmares) or atypical antipsychotics may be used, particularly if symptoms are severe or other treatments have not been effective.
3. Alternative Therapies:
- Mindfulness and Stress Reduction Techniques: Practices such as mindfulness meditation, yoga, and acupuncture can help reduce stress and improve emotional regulation.
- Animal-Assisted Therapy: Interaction with animals, such as service dogs, can provide comfort and reduce anxiety.
4. Self-Care and Support:
- Healthy Lifestyle Choices: Regular exercise, a healthy diet, and sufficient sleep can improve overall well-being and reduce PTSD symptoms.
- Support Networks: Building a strong support system of friends, family, and support groups can provide emotional backing and reduce feelings of isolation.
Treatment plans should be tailored to your needs, and it may take time to find the most effective combination of therapies. It's important if you struggle with PTSD to work closely with healthcare providers to monitor progress and make necessary adjustments to your treatment plan.
Available Help
988 Suicide and Crisis Lifeline We can all help prevent suicide. The 988 Lifeline provides 24/7, free and confidential support for people in distress, prevention and crisis resources for you or your loved ones, and best practices for professionals in the United States.
Find A.A. Near You This website does not contain a meeting finder. Contact one of the A.A. resources below for a meeting list in that location and the surrounding area.
The Online Intergroup of Alcoholics Anonymous, or OIAA, is an International service organization established in accordance with the Ninth Tradition of Alcoholics Anonymous A.A., specifically for the purpose of assisting online.
All of the efforts of Narcotics Anonymous are inspired by the primary purpose of our groups. Upon this common ground we stand committed.
Marijuana Anonymous is a simple program based on one addict helping another.
A simple, supportive approach to mental health care. Find a therapist who fits your needs and takes your insurance.
The United States Department of Veterans Affairs is a Cabinet-level executive branch department of the federal government charged with providing lifelong healthcare services to eligible military veterans at the 170 VA medical centers and outpatient clinics located throughout the country.
NAMI is the National Alliance on Mental Illness, the nation’s largest grassroots mental health organization dedicated to building better lives for the millions of Americans affected by mental illness.
If you or someone you know has a mental illness, is struggling emotionally, or has concerns about their mental health, there are ways to get help.
The Substance Abuse and Mental Health Services Administration (SAMHSA) is the agency within the U.S. Department of Health and Human Services (HHS) that leads public health efforts to advance the behavioral health of the nation and to improve the lives of individuals living with mental and substance use disorders, and their families.
The National Network of Depression Centers (NNDC) develops and fosters connections among members to use the power of our network to advance scientific discovery, and to provide stigma free, evidence-based care to patients with depressive and bipolar illnesses.